Caltech Alumni Leap into Fight Against COVID‑19
By Judy Hill
Spring was finally on the horizon. Two medical interns were in the midst of grueling residencies in busy urban hospitals on the east coast. In Southern California, a radiologist was juggling a lab, a start-up, and a clinical practice, while an emergency medicine physician had her hands full at two local hospitals. On the Caltech campus, a postdoc and a graduate student were engrossed in their bioengineering and chemical engineering research; at JPL, a systems engineer was at work on a mission that aims to collect space-based data to examine how airborne particles affect human health.
Then COVID-19 arrived in the United States and ratcheted up the intensity of their already hectic lives. Driven to respond to this new challenge, these Caltech alumni found ways to apply their knowledge and expertise to join the fight against the disease. They improved testing capabilities, designed face shields, addressed problems of ventilator scarcity, and had the most difficult conversations of their lives.
“I don’t think I could have predicted that our efforts would pan out the way they have,” says Albert Hsiao (BS ’00, biology, engineering/computer science), a cardiothoracic radiologist who developed a machine learning algorithm to detect pneumonia. “But it is what I always hoped would happen: that the things we learned at Caltech, everything that we trained for, can now be applied and have meaning for society.”
A faster, better test
Mikhail Hanewich-Hollatz (PhD ’20, bioengineering) was several months into a bioengineering postdoc appointment in Professor of Applied and Computational Mathematics and Bioengineering Niles Pierce’s Caltech lab when the first rumblings of the coronavirus began to be felt on campus. He remembers that, during the same week in which Pierce sent everyone home to work remotely, his brother emailed him a screenshot of a tweet from Curative, an L.A.-based biotech company, which was looking for people with wet lab experience to volunteer on a project to scale up COVID-19 testing.
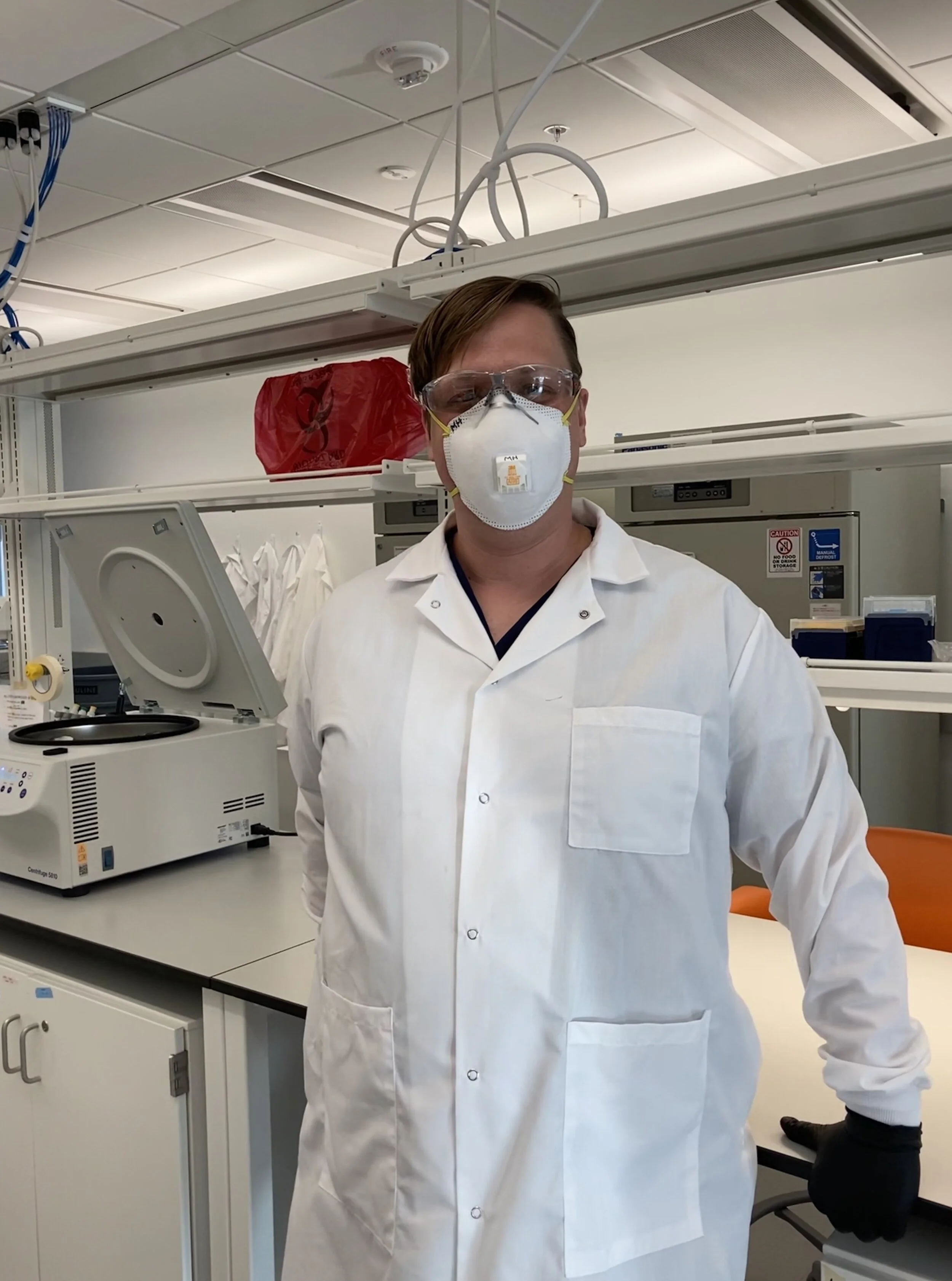
Mikhail Hanewich-Hollatz (PhD ’20)
“And I thought, basically, ‘I have to do this,’” says Hanewich-Hollatz, who is adept at PCR (polymerase chain reaction, a way to make vast numbers of copies of a specific DNA sample) and RNA extraction, both parts of the process of the dominant type of COVID-19 diagnostic test. “‘That’s me; I have those skills. Under what other circumstance is my skill set going to really be able to make a significant impact in a time of crisis?’”
When Hanewich-Hollatz interviewed for a spot and relayed his experience engineering custom RNAs for the genome-editing tool known as the CRISPR/Cas9 system, Curative suggested that rather than being a volunteer tech, pipetting samples, he might be more valuable as an associate scientist on the research-and-development team. So ended Hanewich-Hollatz’s postdoc; in its place began an opportunity he could never have foreseen.
His first job was to help reconfigure the L.A. lab space for COVID-19 diagnostics and then to convince the FDA that the test could be carried out with more readily available materials than those that had been approved at the time and were in extremely short supply.
He and his colleagues also worked to adjust and automate portions of the test for extremely large-scale repetition. The FDA came through with Emergency Use Authorization approval and, in just seven weeks, the lab went from running zero tests a day to 13,000, or approximately 20 percent of all the tests run in the state of California at that time.
Toward the end of March, Hanewich-Hollatz was asked to fly to Washington, D.C., to set up a similar facility. Within 48 hours of landing, he had a functional lab set up. By early May, he had hired 50 people to process patient samples and anticipated that ultimately the lab’s capacity would be around 50,000 tests a day. Recently, he was promoted to Curative’s director of laboratory operations for Washington, D.C.
The most gratifying part of the experience for him has been the immediacy of the impact he has been able to make. “It’s an experience that is very, very different from grad school, where you’re struggling for years and whether you’ve made any real progress is a matter for debate.”
His current role is not something he would ever have envisioned, he says, but it has reshaped what he finds interesting. “What we’re doing here is integrating things in a new way. We’re cutting through some of the bottlenecks. It’s not pushing the boundaries of what’s possible in a single experiment but pushing the boundaries of what’s possible to provide society.”
An algorithm to detect pneumonia
Since the majority of seriously ill COVID-19 patients develop pneumonia, it is important to detect the condition as quickly as possible, even before a definitive COVID-19 diagnosis, says Hsiao. That way, treatment can begin immediately.
Hsiao, a cardiothoracic radiologist at UC San Diego Health, has developed an artificial intelligence (AI) algorithm that can rapidly and accurately highlight areas of pneumonia on an X-ray. “This is useful for less-experienced radiologists as well as physicians who are not radiologists,” he explains. “ER docs and ICU docs who are closer to the point of care might not have as much experience reading the X-rays as a subspecialty radiologist, and the findings of viral pneumonia can be really subtle. With this pandemic, people are doing jobs they weren't necessarily experts in before.”
The Power of AI
Albert Hsiao (BS ’00), a radiologist at UC San Diego Health, developed an AI algorithm to accurately pinpoint areas of pneumonia, a common affliction for coronavirus patients, on an X-ray. Photos: UC San Diego Health
Hsiao had previously developed a 4-D cardiac-imaging software to measure and visualize blood flow with an MRI. When the Society of Thoracic Radiology put out a challenge a year and a half ago to develop a machine learning algorithm to locate pneumonia on an X-ray, he and his lab decided to take a new approach. The algorithm they developed, which was trained with 22,000 annotations by subspecialty radiologists, overlays X-rays with color-coded maps that indicate areas of pneumonia.
When the first reports of a novel coronavirus began to surface last December, Hsiao’s paper on the algorithm, which had been accepted by the Journal of Thoracic Imaging, had yet to be published. “I asked my research resident to download images of chest X-rays from COVID-19 patients from a couple of different journal articles and just try the algorithm out on them to see if it could pick up the pneumonia,” says Hsiao, whose team immediately published a research letter with the results. “It was like magic, it just worked. So, that gave us confidence right away that we should try to deploy this in our clinical practice.”
In late March, UC San Diego Health began using the algorithm, and the results in real-life cases were just as impressive. “We’ve had patients who weren’t initially thought to have COVID come in for abdominal pain and then get an X-ray along the way,” he says, “and the AI has detected their viral pneumonia, which then led to the RT-PCR [reverse transcriptase PCR] test to confirm they had COVID.”
Now Hsiao is working with members of his lab to fine-tune and improve the algorithm, and has initiated collaborations with several other academic medical centers across the United States. Through Arterys, his start-up company, he has also made the initial prototype available on the web so that physicians in hospitals anywhere can try using it with their own X-ray images.
This crisis, Hsiao says, highlights the importance of physician-scientists. “I feel like the role of physician-scientists has been unfortunately fading over the years, and the divide between hospitals and new technologies has grown. Hospitals have shifted to focus on financial concerns, such as revenue and bottom line, while industry often builds technologies without a full understanding of the clinical problems. Physician-scientists are needed in between to bridge the gap between technology and medicine.”
A face-shield assembly line
Dennis Ko (MS ’12, chemical engineering), who is currently pursuing his doctoral degree in chemical engineering at Caltech, was inspired to get involved when his partner, Lisa Yee (BS ’10, biology), an emergency-medicine physician, told him she had to continually reuse her N95 mask and face shield because supplies were so limited. When she finished her shifts at Kaiser Permanente medical centers in Fontana and Ontario, she would stash her face shield in her backpack. After a few weeks of this, the plastic guard was getting crinkly.
With hospitals in Southern California preparing for a surge in COVID-19 cases in March, Yee explains, health-care facilities were trying to conserve their supplies of personal protective equipment for high-risk procedures such as intubations.
Expert assistance
Lisa Yee (BS ’10) and Dennis Ko (MS ’12), designed and printed face shields for area hospitals. Photo courtesy of Lisa Yee and Dennis Ko
“I’d been reading online that a lot of people were 3-D printing their own face shields, and I thought, ‘You know what? I’ll just learn how to do it.’ I talked to my adviser, Julia Kornfield [BS ‘83, Elizabeth W. Gilloon Professor of Chemical Engineering], and she said, ‘Even if you only print five face shields, that’s five people you managed to help.’”
After purchasing an inexpensive 3-D printer and a couple of spools of PLA (polylactic acid, a bioplastic made from lactic acid), Ko and Yee began researching face-shield designs in early April. On the National Institutes of Health (NIH) website, they discovered a 3-D-printing repository with user-submitted designs. “We found one that was clinically reviewed, meaning you can take the shield on and off 10 times without it destructing or losing its quality. So I said, ‘Let’s just go for that one.’”
The first shield took five hours to print and was deemed good but not perfect by Yee. From her frontline experience caring for patients, she realized that a shield with a full brim that fit snugly against the forehead would provide better coverage than the design they had printed, which had a gap at the top. Ko ended up adapting another design from the NIH site using computer-
aided design software. “I think there were a total of 13 iterations,” says Ko. “There was a huge learning curve.”
Once the pair had settled on the optimal design, their operation quickly gathered steam as Yee identified more physicians and nurses in her department, as well as former residency colleagues now at other hospitals, in need of face shields. Ko bought two additional printers and increased his production to 100 masks every three or four days. During April and May, they supplied a total of 600 face shields to medical centers around Southern California.
For Yee, having an extra shield or two gives her an added sense of safety. “Now, with any patient who has a fever, cough, or shortness of breath, I can go into the room with my own face shield. Afterward, I just wipe down the plastic part that goes around the head and change out the transparent plastic shield, and I’m good to go.”
To amplify the impact of the project, which is funded entirely through donations, Ko has uploaded their design to the NIH repository, where anyone can download it for free.
A front-line position
As an internal medicine resident at Columbia University Medical Center, Prakriti Gaba (BS ’13, biology and business, economics, and management), was on the front lines caring for patients with COVID-19 at New York-Presbyterian Hospital from the earliest days of the pandemic.
In the trenches
Prakriti Gaba (BS ’13), an internal medicine resident at Columbia University Medical Center, was on the front lines caring for patients with COVID-19 since the start of the pandemic. Photo: Courtesy Prakriti Gaba
When the first few cases of COVID-19 emerged in the city in mid-March, she began working in the intensive care unit and from there moved on to the emergency room, taking care of many patients who were intubated and required ICU-level care. Since then, she has also worked on the inpatient floors and in new temporary ICUs (rooms converted from medical-surgical units to accommodate the rapid surge in cases).
“As COVID-19 spread in New York City, patients were flooding into the ER,” she says. “Some were really young, in their 20s, without comorbidities, and everyone was extremely sick. Many patients were intubated as soon as they arrived.”
Already accustomed to long hours as a resident, Gaba and her colleagues pushed through punishing schedules with 12-hour days and one day off a week, at most. What she found hardest, though, were the end-of-life discussions with patients’ family members. “It was absolutely heartbreaking,” she says. “No part of me was ready to convey that loved ones can’t talk, hug, or say goodbye to their father, grandmother, or son, or that their loved ones would have to be away from family during their final moments.”
She has felt inspired, though, by fellowship with her colleagues. “What has been the most rewarding aspect of this whole experience is being a part of the immense camaraderie among doctors and nurses from all specialties (orthopedics, dermatology, ENT, and many more) working tirelessly together to tackle this pandemic. It is absolutely remarkable how everyone has teamed up to fight this fight.”
A rapidly deployable ventilator
Elisa Walsh (BS ’12, biology, minor in English), an anesthesia resident at Massachusetts General Hospital, remembers hearing reports in early March about hospital systems in Italy becoming completely overwhelmed with the influx of COVID-19 patients. One detail, the lack of mechanical ventilators, stood out for her.
Elisa Walsh (BS ’12) joined with fellow physicians to launch a global challenge to design a ventilator for use in pandemics. Photo: Massachusetts General Hospital, Department of Anesthesia, Critical Care, and Pain Management
“In our hospital, we’ve seen some COVID-19 patients on a ventilator for weeks while recovering,” she says. “In Italy, the ventilator shortages pressed doctors into making the unimaginable decision of choosing who would get a ventilator and who would not. As an anesthesia resident, I felt an immediate calling because every single day I’m working with mechanical ventilators for patients in the operating room and the intensive care unit. I can’t imagine not being able to provide this lifesaving technology to a patient who is in need.”
Sometime in the middle of March, a senior resident at the hospital proposed pushing out a moonshot challenge to engage people all over the globe to design a ventilator that would be rapidly deployable and could be used in a low-resource setting. Walsh signed on, with a handful of other Mass General residents, and the CoVent-19 Challenge was born, officially launching on April 1, which was also when their hospital received its first real wave of COVID-19 patients. Walsh serves as lead on the medical expert panel of the 19-person team coordinating the initiative.
The typical ICU ventilator is “this extraordinary piece of technology,” says Walsh, “but they’re very big, very complex, and very difficult to manufacture in bulk and store within the hospital.” The ideal ventilator for a pandemic is one that is smaller and simpler in design and able to be quickly manufactured in large quantities.
More than 150 initial entries were submitted by the May 1 deadline; seven from across the globe were invited into the final round. In July, Walsh and her fellow team members selected the winning design to be prototyped and undergo necessary regulatory testing. Though aware that their timeline meant they missed the first months of the pandemic’s spread in the U.S., they hope the winning ventilator will be able to support patients in the future.
A VITAL contribution
In Pasadena, JPL engineers also pivoted to address the ventilator problem and developed a new high-pressure ventilator in just 37 days in March and early April to treat COVID-19 patients. The new ventilator was granted an Emergency Use Authorization by the FDA on April 30. Caltech’s Office of Technology Transfer and Corporate Partnerships offered a free license for the device and reached out to the medical industry to find manufacturers. Almost 100 proposals were submitted to receive the license and so far, 27 companies have received them, nine in the United States and 18 internationally.
JPL engineer Stacey Boland (PhD ’05)
Called VITAL (Ventilator Intervention Technology Accessible Locally), the unit can be built faster and operated more easily than a traditional ventilator and is composed of far fewer parts. The FDA has since awarded a second authorization for a modified design of VITAL that uses a compressor to generate pressurized air, which makes it ideal for a wider range of medical locations, including field hospitals.
JPL engineer Stacey Boland (PhD ’05, mechanical engineering) served as the operations lead for the project, creating a communication pathway between engineers, designers, and visualization specialists with doctors, nurses, and respiratory therapists.
“With systems engineering, some of the time you’re the glue and sometimes you’re the lubricant,” says Boland. “You just try to keep things going, make sure that people communicate with each other. We clearly hit upon a real need and are offering a compelling solution. We’re breaking all sorts of new boundaries in terms of figuring out how to do things in a different way.”
Though Boland knew next to nothing about ventilators at the outset of the project, she says, “You figure it out, and you follow your gut, and you fill in the blanks. You need to be willing to learn and ask questions.”
Even when the ventilator project is behind her, Boland says the pandemic will still factor into her research on airborne particulate matter and health, since many of the preexisting conditions that impact response to the disease can be correlated with air pollution. “The COVID-19 aspect is going to still be there career-wise for me in terms of an interesting area of research,” she says, “and that certainly wasn’t something that I was anticipating.”
Ask a Caltech Expert: Professor Pamela Bjorkman on SARS-CoV-2
In a March 2020 webinar, Pamela Bjorkman, Caltech’s David Baltimore Professor of Biology and Bioengineering, provided an introduction to viruses, antivirals, and vaccines in the context of SARS-CoV-2, the virus that causes COVID-19. Here, she answers questions from the public.
Human Impacts on the Atmosphere as Revealed by COVID-19
Experts from campus and the Jet Propulsion Laboratory (JPL), which Caltech manages for NASA, presented a webinar on June 9, 2020, discussing how changes in energy use, transportation, and manufacturing during the coronavirus pandemic can be connected to changes in air quality and emissions of greenhouse gases, such as carbon dioxide and methane. Panelists discussed how this has created an experiment that can help us understand how human activity changes the environment and guide policies for a transition to a sustainable planet.